High blood pressure is a common condition that affects 45% of all adults in the U.S. As you get older, the risk of high blood pressure increases. The Center for Disease Control (CDC) also breaks down the rates of high blood pressure by gender and race:
Gender: Male-identifying patients (47%), female-identifying patients (43%)
Race: Non-Hispanic black adults (54%) exhibit higher rates than non-Hispanic white adults (46%), non-Hispanic Asian adults (39%), or Hispanic adults (36%)
For many people, there is no cause when it comes to high blood pressure. This type is called primary (essential) hypertension, and it develops slowly over time. There is another type called secondary hypertension, which is caused by an underlying condition. Overall, the risk factors associated with high blood pressure are:
Family history
Obesity / being overweight
Lack of regular exercise
Tobacco use
High-sodium diet
Low-potassium diet
Heavy alcohol use
Recreational drugs (such as cocaine and amphetamines)
Stress
Pregnancy
Chronic conditions (such as sleep apnea, kidney issues, adrenal gland tumors, thyroid issues, and congenital defects in blood vessels)
Prescription and over-the-counter drugs (such as birth control pills, cold medicine, decongestants, and pain relievers)
The majority of people with high blood pressure do not have any symptoms, even when their blood pressure has reached a severe stage. That’s why high blood pressure is known as the “silent killer.”
Some people do report symptoms when they have severe hypertension, such as:
Headaches
Shortness of breath
Nosebleeds
Flushing
Dizziness
Chest pain
Visual changes
Blood in urine
These can be a sign of a severe stage of the disease and require medical attention straight away.
Pharmacist Tip
It is common to require more than one blood pressure medication in order to get your blood pressure under control. For example, elderly and people diagnosed with resistant hypertension may require a combination of up to three or four different medications in order to control their blood pressure.
A common side effect of blood pressure medication can be dizziness. Dizziness can be dangerous, especially for the elderly, since it may lead to falling over and injury. When getting out of bed or a seated position, make it a habit to get up slowly and allow your feet to dangle to the ground for a moment before standing up. This will allow time for your blood pressure to normalize and will prevent dizziness.
It is best to take blood pressure medications around the same time each day. If you are taking blood pressure medications such as hydrochlorothiazide, chlorthalidone, furosemide, or any other “diuretic,” it is recommended to take your daily dose in the morning since these medications may increase urination. Taking them at night may cause you to wake up in the middle of the night to urinate.
Since most people do not see any symptoms or signs of high blood pressure, it is important to get yours checked frequently as part of routine visits with your primary care physician. High blood pressure is easily detected with an arm cuff and pressure-measuring device.
Before diagnosing you, your doctor will likely check your blood pressure three or more times at different appointments. This is because some people will show higher readings during a visit to a doctor, possibly due to nerves (this is called “white coat hypertension”). If your doctor still suspects you might have hypertension, they may order additional tests such as a urine sample, blood test, cholesterol test, electrocardiogram, and/or an ultrasound of your heart or kidneys.
If you are diagnosed with high blood pressure, it is important to regularly take and record blood pressure readings. Keep a log with the date and time, and bring the log with you to your doctor’s appointment for review. There are also blood pressure monitors that have extensive memory to keep track for you. This will help your doctor adjust your medication if necessary and track your progress.
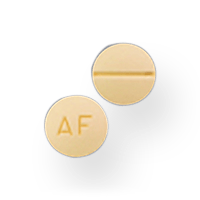
There are four main groups of prescription medications typically used to treat high blood pressure:
Diuretics:
Thiazide diuretics: for example hydrochlorothiazide (Microzide)
Potassium-sparing diuretics: for example Triamterene or Spironolactone
Loop diuretics: like Furosemide (Lasix) or bumetanide (Bumex)
Combination diuretics: combing above diuretic categories like triamterene + hydrochlorothiazide (Dyazide, Maxzide)
Angiotensin-converting enzyme (ACE) inhibitors: lisinopril (Zestril), benazepril (Lotensin), and captopril (Capoten)
Angiotensin II receptor blockers (ARBs): candesartan (atacand), losartan (Cozaar), or valsartan (Diovan)
Calcium channel blockers: amlodipine (Norvasc), Nifedipine (Adalat CC or procardia XL), Diltiazem HCL (Cardizem CD, Cardizem SR, Dilacor XR, Tiazac)
Beta-blockers: like atenolol (Tenormin), metoprolol tartrate (Lopressor), metoprolol succinate (Toprol-XL), propranolol (Inderal)
Alpha blockers: like Doxazosin (Cardura), Prazosin (Minipress), Terazosin (Hytrin)
Alpha-2 Receptor Agonists: Methyldopa
Central Agonists: like clonidine (Catapres), guanfacine (Tenex)
Blood vessel dilators (aka Vasodilators): Hydralazine (Apresoline) or oral Minoxidil (used in severe cases where kidney failure is present)
Not all generics are the same. Different people respond better to different versions of the same drug, depending on the manufacturer. You can search our website to find the best fit for you.
There are some lifestyle changes you can adopt to lower your blood pressure. Try eating a low-sodium, healthy diet and reducing your alcohol and tobacco consumption. Food that is high in salt can cause blood pressure to rise. When we consume too much salt, our body tends to regulate this by retaining more water, which can cause blood pressure to increase. The American Heart Association recommends limiting daily sodium intake to no more than 1,500 mg per day. Reducing salt intake can mean choosing foods that are labeled “low sodium” or “sodium-free,” not adding additional salt to meals, and overall avoiding foods that may be high in salt (i.e. frozen processed foods, processed meats, pickled foods, and potato chips).
Alcohol can also increase blood pressure. The recommendation is to limit alcohol consumption to no more than one drink per day for women and no more than two drinks per day for men. One standard drink is considered either 12 ounces of regular beer (5% alcohol), 5 ounces of wine (12% alcohol), or 1.5 ounces of distilled spirits (40% alcohol).
Regular exercise and maintaining a healthy weight are also important factors for healthy blood pressure levels. It is recommended to engage in at least 150 minutes of moderate-intense aerobic activity per week or 75 minutes of vigorous aerobic activity per week. This can be broken down into smaller sessions over the course of 3-4 days per week. Examples of moderate-intensity aerobic activity include biking, brisk walking, swimming, or even dancing. Vigorous-intensity aerobic activity may include running, jump rope, or hiking.
Lastly, do your best to manage stress levels. Techniques such as deep breathing, meditation, and taking walks might help.